|
:::
 |
 |
 |


|
Minimally Invasive |
 |
What Is Minimally Invasive Spine Surgery? |
|
In essence, minimally invasive spine surgery is the performance of surgery through small incision, usually with the aid of microscopes or endoscopic visualization (i.e., very small devices or cameras designed for viewing internal portions of the body). |
 |
Why Is Minimally Invasive Spine Surgery Needed? |
 |
|
Minimally invasive spine surgery has developed out of the desire to effectively treat disorders of the spinal discs with minimal muscle related injury, and with rapid recovery.
Traditionally, surgical approaches to the spine have necessitated prolonged recovery time. For example, prior to the use of the operating room microscope a large incision was used to visualize the herniated lumbar disc. In order to perform this procedure, large sections of the back muscles are moved away from their spinal attachments.
First, this surgical approach (i.e., dissecting the muscles) produces the majority of the perioperative pain and delays return to full activity. The degree of the perioperative pain necessitates the use of significant pain medication with their inherent side effects. Also, the degree of the perioperative pain delays return to normal daily activities and nonphysical work.
Second, the dissection of the paraspinal muscles from their normal anatomic points of attachment results in a healing by scarring of these muscles. The various layers of the individual muscle scar to one another losing their independent function.
In addition, it has been found that this type of dissection sometimes results in the loss of innervation (i.e., the supply of nerve stimulation) of the muscles with subsequent wasting away. A permanent weakness of the back muscles results. This weakness itself may be symptomatic (as a back fatigue-type pain) and/or limit the patient's function - particularly in those who perform physical work.
Clearly, with such significant muscle injury associated with surgical approaches to the spine, the need existed for the development of less invasive surgical techniques. It was envisioned that minimally invasive techniques would offer several advantages including: -Reduced surgical complications - Reduced surgical blood loss - Reduced use of post-op narcotic pain medicines - Reduced length of hospital stay - Increased speed of functional return to daily activities
Thorascopic, laparoscopic, endoscopic, "through the scope", minimally invasive? These terms describe recently popularized approaches to spine surgery. In order to understand how these approaches may have a role in your spinal surgery, the terminology must be understood.
? |
 |
Endoscope |
|
 An endoscope is an instrument used for the examination of a hollow viscus such as the bladder or a cavity such as the chest. The endoscope is basically a camera mounted on a long thin lens with a cable and a light source. The light source is mounted onto the lens and provides light to illuminate the field to be visualized. The cable mounted on the camera connects to a TV screen, which displays the camera's field of focus. An endoscope is an instrument used for the examination of a hollow viscus such as the bladder or a cavity such as the chest. The endoscope is basically a camera mounted on a long thin lens with a cable and a light source. The light source is mounted onto the lens and provides light to illuminate the field to be visualized. The cable mounted on the camera connects to a TV screen, which displays the camera's field of focus.
|
 |
Endoscopy, Thorascopy, Laproscopy |
 |
|
 Endoscopy is the visual inspection of any cavity or hollow viscus by means of an endoscope. Thorascopy is the visualization of the thoracic cavity or the chest. Thorascopy is used to assist in procedures on the heart and lungs. Laproscopy is the visualization of the abdominal cavity. Laproscopy is used to assist in procedures on the intestines, stomach, or removal of the gallbladder. Endoscopy is the visual inspection of any cavity or hollow viscus by means of an endoscope. Thorascopy is the visualization of the thoracic cavity or the chest. Thorascopy is used to assist in procedures on the heart and lungs. Laproscopy is the visualization of the abdominal cavity. Laproscopy is used to assist in procedures on the intestines, stomach, or removal of the gallbladder.
What is the purpose of utilizing the endoscope? The endoscope allows the surgeon to have an illuminated and magnified view of the operating field without having to make a large incision. With the assistance of the endoscope surgeons can utilize several small incisions to perform the same procedure they would otherwise perform using a single large incision.
Laproscopic and thorascopic surgery are not new techniques. Dr. Jacobaeus was the first to publish his work in 1910 on both of these topics. In the 1980's laparoscopic cholescystectomy or removal of the gallbladder became very wide spread. However, it was not until the early 1990's when the application of these techniques became utilized in the field of spinal surgery. Early uses were for biopsy, removal of thoracic disc herniations and releasing or mobilizing the anterior spine for Scoliosis and Kyphosis. The applications rapidly expanded to many aspects of spinal surgery. |
 |
Instrument Availability |
|
Unfortunately just the existence of the endoscope does not automatically allow the spine surgeon to perform surgery endoscopically. First, the surgeon must first recognize if the surgery can be performed without a formal incision. Currently only a small number of spinal surgeries can be performed utilizing an endoscopic approach. Once deciding to perform the surgery endoscopically, the surgeon must determine if all of the instruments and implants (screws, rods, and cages) are available to perform the surgery. You may ask, if the surgery is now being performed with a formal incision, are not all of the tools and implants needed to perform the surgery already available? The answer to this is unfortunately no. Instruments used for endoscopic surgery differ from the instruments used to perform surgery through a formal incision. |
 |
Endoscopic Instruments |
 |
|
 When a surgery is performed with a large incision the dissection leads the surgeon directly to the spine. The approach enables the surgeon to touch the spine and manipulate the spine manually as is often necessary. Instruments for performing open surgery are traditionally made short allowing the surgeon better control and tactile feel. The implants and the tools used to insert the implants are often very large and bulky, because the incision size allows a large access. When a surgery is performed with a large incision the dissection leads the surgeon directly to the spine. The approach enables the surgeon to touch the spine and manipulate the spine manually as is often necessary. Instruments for performing open surgery are traditionally made short allowing the surgeon better control and tactile feel. The implants and the tools used to insert the implants are often very large and bulky, because the incision size allows a large access.
In developing the endoscopic approach for spinal surgery, the first task was to develop longer streamlined instruments. New and different instruments needed to be developed to perform tasks that were normally done with the surgeon's hands on the spine, but now must be performed at a significant distance from the spine. As these instruments were developed basic procedures could now be performed endoscopically. As the technique progressed the desire to instrument the spine became the next step. We needed to develop implants that could fit through small incisions and the instruments to insert and manipulate the implants that would fit through the same portals.
 Portals are devices that provide a passage through which the surgeon operates. The incisions for endoscopic surgery are usually a centimeter in length. Once the skin incision is made an instrument is used to continue the dissection into the cavity, usually the chest or abdomen, depending the incision location and the patient's body this can be a fairly long distance. When the instrument is removed all the tissue falls back into place and the opening into the cavity can be very difficult to find. In order to avoid damaging the tissue by moving instruments in and out of the passage, a portal is placed into the incision to hold the tissue apart Portals are devices that provide a passage through which the surgeon operates. The incisions for endoscopic surgery are usually a centimeter in length. Once the skin incision is made an instrument is used to continue the dissection into the cavity, usually the chest or abdomen, depending the incision location and the patient's body this can be a fairly long distance. When the instrument is removed all the tissue falls back into place and the opening into the cavity can be very difficult to find. In order to avoid damaging the tissue by moving instruments in and out of the passage, a portal is placed into the incision to hold the tissue apart
There are two main designs of portals, open or sealed. The open portal is an open tube that allows for the passage of air from outside of the body to inside the cavity and acts only as a spacer. The sealed portal limits the passage of air or gas into or out of the cavity. This type of portal is often used in the abdominal cavity, this allows for the cavity to be expanded allowing the surgeon space to operate. The portals used in the thoracic spine tend to be 11 to 12mm, while portals used in the abdominal cavity tend to be larger. All of the instruments and implants had to be made to not only fit through these small passages, but also perform their function once inside the cavity. |
 |
Operating Space |
 |
|
 In the thoracic spine the space to operate through is provided by deflating the lung. The anesthesiologist performs this by placing a special breathing tube down the trachea into the large airway of each lung. Once in place the patient is asleep and breathing with only one lung, which is very safe and commonly done. This allows the opposite lung to deflate and falls out of the way of the spine. The portals are placed and the procedure to be performed on the spine is begun. While in the thoracic cavity the lung is collapsed for space, in the abdomen the cavity is filled with CO2 gas creating the operating space. In the thoracic spine the space to operate through is provided by deflating the lung. The anesthesiologist performs this by placing a special breathing tube down the trachea into the large airway of each lung. Once in place the patient is asleep and breathing with only one lung, which is very safe and commonly done. This allows the opposite lung to deflate and falls out of the way of the spine. The portals are placed and the procedure to be performed on the spine is begun. While in the thoracic cavity the lung is collapsed for space, in the abdomen the cavity is filled with CO2 gas creating the operating space.
The goal of endoscopic surgery must be the same as surgery performed with a formal open procedure. The incision and tissue dissection to the spine may be less, but the surgical procedure cannot be less. Advantages of endoscopic surgery include: improved postoperative recovery, decreased pain, and faster return to activities. These findings have been demonstrated in many, but not all endoscopic procedures. Even today only a small percentage of spinal conditions are suitable for endoscopic surgery. Do not hesitate to discuss with your spine surgeon if your particular condition is amenable to an endoscopic approach. |
 |
Microendoscopic Discectomy |
 |
|
The Microendoscopic Discectomy (MED) is a minimally invasive surgical technique used to remove a herniated disc. When a nerve is compressed by the disc it can cause symptoms such as extremity pain, numbness, weakness, electrical sensations, and bowel and bladder incontinence. If symptoms are not relieved with conservative treatments, a patient may be a candidate for surgical removal of the herniated disc fragment.
Microendoscopic Discectomy differs from the open microdiscectomy. The incision using the microendoscopic technique is smaller (approximately 1cm), causing less trauma to the surrounding tissue. A smaller incision allows for decreased post-operative pain and a faster recovery. A patient is considered a potential candidate for a microendoscopic discectomy if he or she has a large herniated disc fragment extruded to the side of the spinal canal.
Microendoscopic Discectomy is performed by making a small incision in the patient's back and inserting a small endoscopic probe between the vertebrae and into the herniated disc space. A small camera is placed through the probe enabling the surgeon to view the operation on a TV screen in the operating room. Small surgical devices are placed through the probe to remove bone and herniated disc fragments. |
 |
Arthroscopic microdiscectomy |
 |
|
Minimally invasive operations are being increasingly used in selected cases as an alternative to traditional surgery for treatment of herniated lumbar intervertebral discs and symptomatic lumbar disc disease. Different techniques and instrumentation have been used including chemonucleolysis (CNL), percutaneous lumbar discectomy (PLD), arthroscopic microdiscectomy (AMD), automated lumbar discectomy (nucleotomy), percutaneous laser disc decompression (PLDD), radiofrequency thermal coagulation (RFT) and intradiscal electrothermal therapy (IDET). These procedures share several advantages over open discectomy. Patients are awake during the procedure, given only light sedation, and are anesthetized with only local anesthesia. The patient is discharged home the same day and allowed to ambulate. Minimal morbidity occurs, as there is no violation of the spinal canal. Also, no bony or ligamentous elements are removed which might result in subsequent segmental instability and no significant epidural or peri-neural scaring when compared with open technique. These advantages translated into shorter recovery time, fewer complications, and satisfactory surgical outcome.
Arthroscopic Microdiscectomy for the treatment of symptomatic disc herniation share a common physical principle which is in a closed compartment like the inter-vertebral disc a small decrease in intradiscal volume will result in disproportional large drop in intradiscal pressure. Central decompression might result in regression of a contained disc herniation and relief of mainly radicular symptoms due to neural compression. Other factors induced by these techniques play a major role in reducing symptoms not only the radicular symptoms but also back pain. The combination of techniques enables the operating surgeon to treat larger herniations, not amenable to central decompression, by targeting the herniation site under direct vision. In addition the back pain component of internal disc derangement can be ameliorated by radiofrequency probes and intradiscal thermoelectric catheters.
A combined technique of percutaneous laser disc decompression and arthroscopic microdiscectomy was used to treat symptomatic lumbar disc herniations. The procedure provides better decompression and can target the herniated fragment under direct arthroscopic visualization. Patients who presented with predominantly back pain had less successful resolution of their symptoms than those who presented primarily with sciatica. |
| |
 |
 |
Kyphoplasty |
 |
|
Spinal compression fractures are a common cause of back pain, spinal deformity and reduced quality of life in elderly patients. These fractures cause the spinal column to shorten and tilt forward. Osteoporosis is the most common cause for spinal compression fractures. Osteoporosis weakens bone architecture and cause compression fractures to occur in the spine.
Spine compression fractures due to osteoporosis cause sudden onset of back pain with little or no trauma. Chronic symptoms include loss of height, spinal deformity and protuberant abdomen. Traditionally, medical treatment of painful osteoporotic compression fractures consists of bed rest, narcotic medications and bracing. These medical treatments are not without problems. While some patients improve with simple measures and time, many others do not. Pain may result in the need for chronic narcotics. Back braces are uncomfortable. Prolonged bed rest is poorly tolerated in the elderly due to medical problems such as blood clots, pneumonia and skin ulcers. Standard open surgery is not recommended due to poor outcomes.
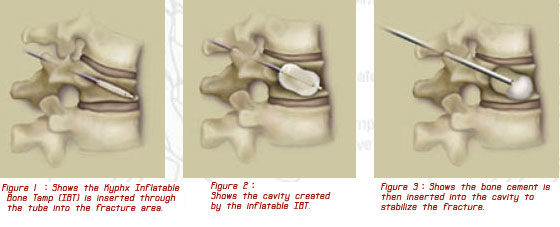
Kyphoplasty is a new treatment option for patients with painful osteoporotic compression fractures. The kyphoplasty procedure is performed by inserting a balloon into the fractured vertebra through a small stab wound on the back. The balloon is inflated to restore the normal height of the vertebral body. Cement is then injected into the vertebra to stabilize the fracture
In addition to the reduction of fracture-related pain, some or all of the height is restored to the compressed vertebral body. Normalizing the height of the fractured vertebra reduces the focally exaggerated curvature of the spine (ie, kyphosis). This effect, in turn, results in an esthetic improvement, improved posture, and a reduced risk of fracture of the adjacent vertebra as a result of abnormal load bearing. The restoration of a more normal appearing configuration of the vertebral body and improvement in the load-bearing physics is accomplished with the intravertebral inflation of 1 or 2 high-pressure balloon tamps.
The kyphoplasty procedure is minimally invasive and performed with limited surgery time. Only one day of hospitalization is required. Recovery is short and patients immediately return to their usual activities of daily living. A brace is not required.
Results of Kyphoplasty are over 90% good to excellent. Results are best for acute fractures less than 3 months old, but even patients with chronic or old fractures can benefit from the procedure. |
| |
 |
 |
Intradiscal Electrothermal Therapy |
 |
|
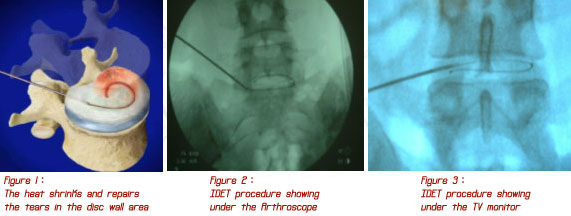
Intradiscal electrothermal therapy (IDET) is a procedure developed to treat the lower back pain associated with contained lumbar herniated discs with annular disruption. The severity of the degenerative disc disease is determined by MRI scanning and discogram.
The primary indications for IDET are patients with back pain reproduced by provocative discography, normal neurological exam, MRI scans demonstrating no neural compression, and failure of standard conservative spine therapy. Absolute clinical results have not been fully elucidated, however, preliminary results are of interest.
During the IDET procedure, the patient is awake, laying on his or her side. An electrode is inserted into the symptomatic disc and gradually heated. The heat causes shrinkage of the outer disc fibers and also deadens the nerve endings going to the disc.
This procedure is somewhat controversial. Earlier studies claimed greater than 70% of patients had improvement of discogenic low back pain after IDET treatment, but more recent studies have shown less than 40% of patients have any improvement or satisfaction after the IDET procedure. This procedure will likely become obsolete in the near future after further independent studies are completed. |
| |
 |
 |
Radiofrequency |
 |
|
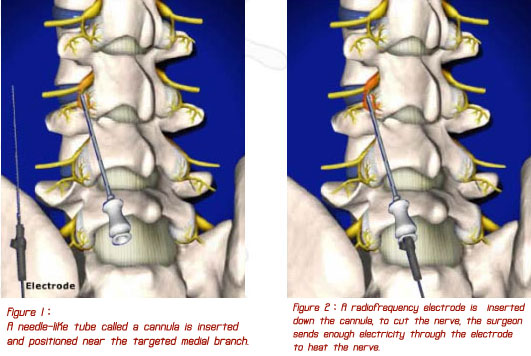
Radiofrequency (RF) lesioning is fast becoming a technique used not only for the destruction of the nerves in the annulus, but also the nerves which innervate the facet joints of the spine. Theoretically, if cervical or lumbar pain can be determined to be emanating from the facet joint pathology, then destruction of the medial branch nerves to the facet joints may eliminate the pain at least temporarily. Specifically, this technique coagulates the medial branch nerves to the facet rendering the joint temporarily anesthetized rather than correcting the underlying pathological disorder. It is a commonly held clinical belief that spinal extension induced pain indicates facetogenic pain. This type of pain is hypothesized to be caused by flexion-extension trauma, progressive arthritis, disc degeneration with a change in spinal weight disruption, or perhaps deterioration of areas above or below fused spinal segments secondary to increased stress in the area of movement.
Radiofrequency facet denervation (also known as facet neurotomy, facet rhizotomy, or articular rhizolysis) is covered for treatment of patients with intractable cervical or back pain with or without sciatica in the outpatient setting when ALL of the following are met:
A. Patient has experienced severe pain limiting activities of daily living for at least 6 months; and
B. Patient has had no prior spinal fusion surgery; and
C. Neuroradiologic studies are negative or fail to confirm disc herniation; and
D. Patient has no significant narrowing of the vertebral canal or spinal instability requiring surgery; and
E. Patient has tried and failed conservative treatments such as bed rest, back supports, physiotherapy, correction of postural abnormality, as well as pharmacotherapies (e.g. anti-inflammatory agents, analgesics and muscle relaxants);and
F. Trial of facet joint injections has been successful in relieving the pain.
|
| |
 |
 |
Laparoscopic Anterior Lumbar Interbody Fusion |
 |
|
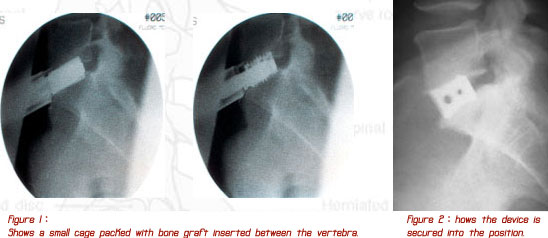
A spinal fusion is the operation performed for the surgical treatment of disabling low back pain that is unresponsive to conservative care. Traditional spinal fusions are done through the back with metal screws and rods or through the abdomen using a large incision. While both approaches have met with reasonable success, many patients are left with back pain and fatigue due to muscle scarring from the operation. The laparoscopic approach is an exciting new procedure done through the abdomen using several small incisions each less than 1" in length. The spine is approached using special instruments and scopes allowing for the placement of two cylindrical dowels made from donor bone. A small amount of bone is taken from the patient's pelvis and packed into the dowels. This allows bone to grow through the implants fusing the vertebral bodies and relieving the patient's back pain.
There are significant benefits to this approach including less post-operative pain, a shorter hospital stay (usually one night), and faster recuperative time. Return to work is possible within weeks of the procedure depending on the requirements of the job. |
| |
 |
|
 |
|
 |