|
:::
 |
 Now:Home page > Spine Disease > Osteomyelitis Now:Home page > Spine Disease > Osteomyelitis |
|
 |
 |

 |

|
Osteomyelitis |

|
Vertebral osteomyelitis refers to an infection of the vertebral body in the spine. It is a fairly rare cause of back pain, especially in young healthy adults.
Generally, the infection is spread to the vertebral body by a vascular route. The veins in the lower spine (Batson's plexus) drain the pelvis and provide for a direct route of entry for the bacteria to get into the spine. For this reason, there is a preponderance of infections in the spine that occur after a urologic procedure (e.g. cystoscopy)
|

|
Causes |

|

|
|
Patients susceptible to osteomyelitis include: |
|
| |
Intravenous drug abuse is a growing cause of spinal infections. Typically, the organism most likely to infect the spine is Staphylococcus Aureus, but in the intravenous drug population, Pseudomonas infection is also a common cause of spinal infection. The treatment for these two pathogens requires different antibiotic therapy.
In the past, tuberculosis infections caused by Mycobacterium Tuberculosis were very common. In North America, this type of infection is not common anymore, but it remains a common organism and cause of spinal infections in countries where there is a lot of poverty. Intravenous drug users are more likely than other patients to contract Mycobacterium Tuberculosis.
Most vertebral body infections occur in the lumbar spine because of the blood flow to this region of the spine. Tuberculosis infections have a predilection for the thoracic spine, and intravenous drug abusers are more likely to contract an infection of the cervical spine. |

|
Symptoms |
| |
Symptoms of back pain due to a spinal infection often develop insidiously and over a long period of time.
In addition to back pain, symptoms may include constitutional symptoms such as: |
- Fever, chills, or shakes
- Unplanned weight loss
- Nighttime pain that is worse than daytime pain
A spinal infection rarely affects the nerves in the spine. However, the infection may move into the spinal canal and cause an epidural abscess, which can place pressure on the neural elements. If this happens in the cervical or thoracic spine, it can result in paraplegia or quadriplegia.
|
| |

|
Diagnosis |
| |
A diagnosis of spinal infection is difficult to make early on in the course of the disease. If osteomyelitis is suspected, both diagnostic studies and laboratory studies will be conducted to make an accurate diagnosis. Sometimes, a surgical procedure may also be necessary to obtain a culture of the bacteria. |
| |

|
Diagnostic studies |

|

|
| |
The process of diagnosing a spinal infection usually starts with an x-ray. X-rays will usually be normal in the first 2 to 4 weeks after the infection starts. For changes to show up on an x-ray, 50% to 60% of the bone in the vertebral body needs to be destroyed. If the disc space is involved (discitis), the disc space may narrow and destruction of the endplates around the disc may be seen on the x-ray.
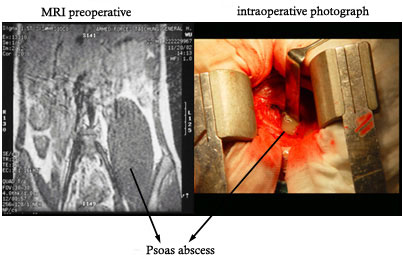
The most sensitive and specific imaging study for spinal infection is a MRI scan with enhancement with an intravenous dye (Gadolinium). The infection will cause an increase in blood flow to the vertebral body, and this will be picked up by the Gadolinium, which will enhance the MRI signal in areas of increased blood flow.
Older tests that are not as specific, such as bone scans, are still sometimes useful, especially if the patient cannot have a MRI scan. Bone scans are fairly reliable in determining if there is increased bone turnover in the spine, but cannot differentiate infection from tumor, trauma, or sometimes even normal degenerative changes. |

|
Laboratory studies |

|

|
| |
Laboratory studies should also be obtained. Blood cultures may pick up the causative organism and help guide antibiotic therapy. Blood cultures are positive probably less than half the time, but when they are positive, they can be a very useful adjunct to guide the treatment (e.g. some bacteria are more sensitive to certain antibiotics than others).
Inflammatory markers can help indicate whether or not there is an infection. The erythrocyte sedimentation rate (ESR) and the C-reactive protein (CRP) are the two best known markers for inflammation, and they will be elevated in 80% to 90% of patients with osteomyelitis.
If these markers are normal, it is very unlikely that the patient has an infection.
If these markers are elevated, it can also serve as a baseline, and subsequent test of these markers will indicate whether or not the patient is responding to a particular therapy. If the markers fall during treatment, then the treatment is likely to be successful in irradicating the infection. |

|
Surgery |
| |
Surgery is sometimes necessary to obtain cultures for diagnosis of which type of bacteria are the cause of the infection. A biopsy may be obtained by needle biopsy, using a CT scan to visualize the needle and guide it into the infection. On occasion, open biopsy may also be necessary for diagnosis. |

|
Treatments |
| |
Treatment for osteomyelitis is usually conservative and based primarily on use of intravenous antibiotic treatment. Occasionally, surgery may be necessary to alleviate pressure on the nerves, clean out infected material, and/or stabilize the spine. |

|
Conservative treatments |
| |
Treatment for spinal infections usually includes a combination of intravenous antibiotic therapy, bracing and rest.
Most cases of vertebral osteomyelitis are caused by Staphyloccocus Aureus, which is generally very sensitive to antibiotics. The intravenous antibiotic treatment usually takes about four weeks, and then is usually followed by about two weeks of oral antibiotics. For infection caused by tuberculosis, a year of oral antibiotic treatment is often necessary.
Bracing is recommended to provide stability for the spine while the infection is healing. It is usually continued for 6 to 12 weeks, until either a bony fusion is seen on x-ray, or until the patient's pain subsides. A rigid brace works best and need only be worn when the patient is active. |

|
Surgical treatments |

|

|
| |
Surgical decompression is necessary if an epidural abscess places pressure on the neural elements. Because surgical decompression often destabilizes the spine further, instrumentation and fusion are also frequently included to prevent worsening deformity and pain.
If the infection does not respond to antibiotic therapy, surgical debridement and removal of infected material may be necessary. Most infections are predominantly in the anterior structures (such as the vertebral body) and the debridement is best done through an anterior (front) approach. Stabilization and fusion are also done after removing the infected bone.
Surgery may also be necessary if there is a great deal of bony destruction with resultant deformity and pain. Reconstructing the bony elements and stabilizing the spine can help reduce pain and prevent further collapse of the spine. The surgery usually needs to be done from a combined anterior (front) and posterior (back) approach.
Most surgeons prefer not to place instrumentation in the front of the spine, where most of the infection is located. If the bacteria set up around inserted hardware, it can then form a covering over itself that protects it from antibiotics. If this happens, the hardware needs to be removed to irradicate the infection.
Bone grafting for anterior column support is usually followed by posterior instrumentation, which places the hardware in a relatively clean environment and decreases the chance of a bacterial infection around the hardware. |
| |
 《Press the button to see the surgical example》 《Press the button to see the surgical example》
|
|
|
 |