| |
Purpose. Current surgical options for osteoporotic kyphosis involve a risk of complex surgery in elderly patients, graft problems (eg, graft dislodgement, subsidence, pseudoarthrosis), and instrumentation problems (eg, adjacent-segment failure, implant pullout). This study is to assess the effectiveness of apical lordosating osteotomy (ALO) and minimal segment fixation through a posterior approach for correcting thoracic or thoracolumbar osteoporotic kyphosis.
Methods. Thirty-two consecutive patients (average age, 71.1 years; range, 65-81 years) with thoracic or thoracolumbar osteoporotic kyphosis underwent ALO. Mean follow-up was 3.2 years (range, 2.1-6.1 years). Radiographic studies, complications, and patient satisfaction were assessed.
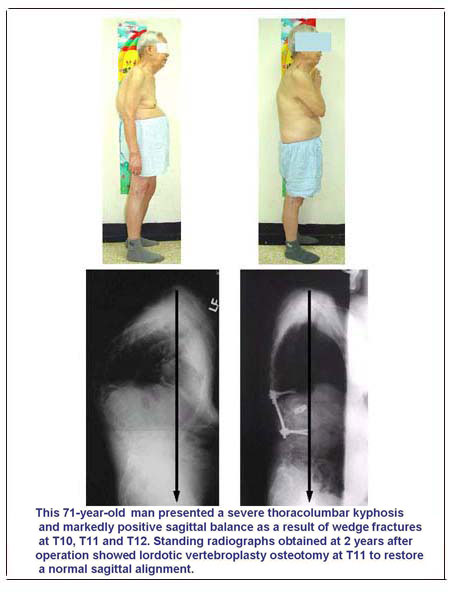
Results. Mean operative time was 135 min, and mean blood loss was 722 mL. In 11 patients with thoracic hyperkyphosis, the mean Cobb angle was corrected from 81.6 ° (range, 73 ° -97 °) to 24.3 ° (range, 18 ° -30 °), indicating normal kyphosis. In 19 patients, thoracolumbar kyphosis of 54.4 ° (range, 45°-71°) was corrected to -2.3 ° (range, -11 ° to 8 °). Sagittal imbalance was 11.5 cm before surgery and 4.8 cm after. Satisfactory correction was achieved in all patients, without anterior release. Local kyphosis was corrected to -9.3 ° from 51.2 °, and mean vertebral kyphosis, to -25.3 ° from 15.6 °. In 17 patients with neurologic deficit, Frankel grades improved postoperatively. No major complication occurred. All patients reported improved pain and self-image and overall satisfaction.
Conclusions. ALO and minimal segments fixation is effective for managing thoracic or thoracolumbar osteoporotic kyphosis. It obviated anterior procedures and had fewer complications and high patient satisfaction.
 《Press the button to see the surgical example》 《Press the button to see the surgical example》
|