|
:::
 |
 |
 |
 |

|
Traumatic Kyphosis |

|

|
|
Compression fractures of the spine are one of the more common injuries sustained by a vertebral structure. The vertebral body itself is the largest single unit of a vertebra. Its structural integrity is similar to a cardboard box.
Imagine a cardboard box; big and sturdy in appearance, but hollow on the inside. Now, let's say a great deal of pressure is placed on this box (vertebral body). Perhaps a hyperflexion injury occurs. In this case, hyperflexion means the neck or low back is forced to bend too far forward or sideways. The result? A crushing effect causes the box (vertebral body) to resemble a wedge. The amount of force delivered to each vertebra is shared directly with the surrounding spinal elements. It might be assumed the smaller cervical vertebrae would be more susceptible to injury simply based on size. Injury of this type generally does not occur often in the lumbar region, due to the size and density of the lumbar vertebrae.
Other fractures can occur from forces that cause the body to torque (twist). Even a direct blow to the spine can cause a fracture. Other parts of the vertebra such as the facet joints, or other bony processes, can break possibly causing dislocation of a vertebra and, perhaps, paralysis to some body part. Although bone is a hard material, it can crack, split, or break away from the parent bone. Spinal fractures require immediate medical attention. An unstable fracture may be a serious condition causing one or more bone fragments to press against the spinal cord or nerves. |
|

|
Severe Pain |
|
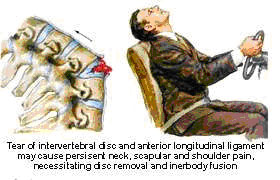 A severe compression fracture may be such that the spinal cord or nerve roots are involved, as they are draped over the sudden angulation of the spine. This may cause severe pain, a hunched forward deformity (kyphosis) and rarely neurologic deficit from spinal cord compression. A severe compression fracture may be such that the spinal cord or nerve roots are involved, as they are draped over the sudden angulation of the spine. This may cause severe pain, a hunched forward deformity (kyphosis) and rarely neurologic deficit from spinal cord compression.
|

|
Risks - Osteoporosis - Trauma |
| |
The risk for spinal compression fracture increases with age. Osteoporosis is the most common risk facture for compression fractures. Osteoporosis is a condition in which there is thinning of the bones, weakening them. This may be due to a lack of calcium in the diet, certain medications, old age, inactivity or genetic factors.
In general, some trauma occurs with each compression fracture. In cases of severe osteoporosis, the trauma may be minimal, such as, stepping out of a bathtub or lifting a heavy object. Moderate trauma is usually required to create a fracture in patients with mild to moderated osteoporosis. This may range from falling off a chair to an automobile accident. A normal spine may also suffer from a compression fracture when there is a severe forward bending injury. This most commonly occurs from a fall from a height or an automobile accident.
|

|
Nerve Injury |
| |
Neurologic injury is rare with compression fractures. The degree of neurologic injury is usually due to the amount of force present at the time of injury. If there is severe angulation of the spine secondary to a wedge fracture, this may stretch the spinal cord and create injury. This would then lead to loss of strength and sensation, as well as reflexes. In most patients with osteoporotic compression fractures, there is no neurologic injury but only pain from the fracture. However, if left untreated the fracture angulation may worsen and lead to late paralogic injury.
|

|
Diagnosis |

|

|
| |
A compression fracture is usually diagnosed by the history, physical exam and x-rays. In any patient over the age of 60 with the acute onset of sudden low back pain, a compression fracture should be suspected. Physical exam will usually note tenderness directly over the area of pain as well as mild kyphotic deformity (e.g., a sudden angulation forward or hunched over appearance). Plain x-rays will demonstrate the wedge shape of the vertebral body on a lateral view. A CAT scan is occasionally needed to help differentiate a compression fracture from a burst fracture.
Occasionally an MRI scan is obtained to rule out disc herniation along with a compression fracture. MRI scan may also help differentiate pathologic compression fractures, that is, those that involve a tumor, from a typical osteoporotic compression fracture. In any patient with a known history of cancer, a compression fracture should tip off the physician to look for evidence of a metastatic lesion and pathologic fracture.
If osteoporosis is suspected, a Bone Mineral Density (BMD) test may be ordered. This test helps determine the severity of the bone thinning. In addition, laboratory tests to look at blood count and thyroid function may be indicated as well. A decision as to whether to treat osteoporosis should be made by the patients' primary physician.
|

|
Treatment |
| |
The majority of mild to moderate compression fractures are treated with immobilization in a brace or corset for a period of six to twelve weeks. The duration of treatment is based on symptoms and x-ray. As pain subsides and x-rays show no change in the position of the spine and healing of the fracture, the brace may be discontinued.
The purpose of the brace is two-fold. Bracing helps to reduce acute pain by immobilizing the fracture. It also helps to reduce the eventual loss in height and in angulation from the fracture. Compression fractures treated in a brace tend to have less deformity than those treated without a brace. Occasionally, bracing beyond twelve weeks is indicated in those patients with severe osteoporosis.
|

|
Stabilization and Fusion |
| |
In most cases, surgery consists of stabilization of the affected portion of the spine. This can be performed with rods and hooks placed from the posterior (back) of the spine. Occasionally the procedure may be performed anteriorly (from the front) to remove the broken vertebra and replace it with a plate, screws or cage.
Either of these approaches involves a spinal fusion of the broken vertebra and its adjacent segments.
|

|
Surgery |
| |
Percutaneous Vertebroplasty is a new surgical procedure that may be used to treat compression fractures in senile patients. In this procedure, the physician or surgeon advanced a catheter into the compressed vertebra under an anesthetic. This catheter is then used to inject the fractured vertebrae with bone cement. This bone cement hardens within the fractured vertebrae and gives the initial stability to the vertebral body. This procedure may be indicated in cases of severe. Spinal surgery is rarely indicated for patients with compression fracture. Indications would include severe fracture with neurologic injury, severe angulation, failure to heal with initial bracing, increased angulation despite bracing or late increasing neuologic deficit. Specific details of indication and type of surgery should be obtained from your personal orthopaedic surgeon.
|

|
Recovery |
| |
Most patients can expect to make a full recovery from their compression fracture. Typically, braces are worn for six to twelve weeks followed by three to six weeks of physical therapy and exercise. This is to help regain strength of the trunk muscles and to increase endurance of the trunk musculature. Overall strength, aerobic capacity and flexibility are also helped by physical therapy.
Most patients can return to a normal exercise program six months after suffering their compression fracture. Regular exercise is one of the activities recommended to help prevent compression fractures in the future. A well-balanced diet, calcium supplement and occasionally other medications prescribed by your personal physician may be needed to help treat osteoporosis.
|

|
Reference Materia |
- Kao-Wha Chang. Anterior Decompression and Fusion for old traumatic cervical cord lesion. J orth Surg ROC 7:53-62, 1990.
- Kao-Wha Chang. A Reduction-Fixation system for Unstable Thoracolumbar Burst Fracture spine. 17:879-86, 1992.
- Kao-Wha Chang. Oligosegemental Correction of post- traumatic Thoracolumbar angular kyphosis spine. 18:1909-15, 1993
 《Press the button to see the surgical example》 《Press the button to see the surgical example》
|
|
 |
|
 |